Understanding Highmark Prior Authorization
The Highmark Prior Authorization Form PDF is essential for ensuring coverage of certain medical services or drugs․ It streamlines the approval process, ensuring quality care while managing costs effectively for patients․
What is Prior Authorization?
Prior authorization is a process where healthcare providers must obtain approval from Highmark before delivering certain medical services or prescribing specific medications․ This ensures that treatments are necessary, appropriate, and cost-effective․ It helps control healthcare costs and prevents unnecessary treatments․ The Highmark prior authorization form PDF is used to request this approval․ Providers submit patient details, treatment plans, and medical justifications․ Highmark reviews these to determine coverage eligibility․ This step ensures evidence-based care, improving patient outcomes while managing financial aspects․ Delays can occur without proper documentation, so accurate and timely submissions are crucial․ Overall, prior authorization balances quality care with cost management, making it essential for both providers and patients to understand and comply with the requirements․
Importance of Prior Authorization in Healthcare
Importance of Prior Authorization in Healthcare
Prior authorization plays a vital role in ensuring that medical treatments are both necessary and cost-effective․ It helps prevent unnecessary procedures, reducing healthcare costs while maintaining quality care․ By reviewing requests, Highmark ensures that treatments align with evidence-based guidelines, improving patient outcomes․ This process also safeguards against inappropriate drug use, minimizing risks and adverse effects․ For providers, prior authorization streamlines communication with payers, clarifying coverage criteria․ Patients benefit from knowing that their treatments are approved and covered, avoiding unexpected medical bills․ Overall, prior authorization strikes a balance between cost control and quality care, making it a cornerstone of modern healthcare management․
The Highmark Prior Authorization Form PDF is essential for obtaining pre-approval of specific treatments, ensuring quality care while managing costs․ It’s downloadable, user-friendly, and required for efficient processing of requests․
Overview of the Highmark Prior Authorization Form
The Highmark Prior Authorization Form PDF is a structured document designed to streamline the approval process for specific medical services or medications․ It collects essential patient and provider information to ensure that treatments meet Highmark’s coverage criteria․ The form typically includes sections for patient demographics, provider details, procedure codes, and clinical justification for the requested service․ By requiring this form, Highmark aims to ensure that treatments are medically necessary and cost-effective, promoting quality care while managing healthcare expenses․ Providers must accurately complete and submit this form to facilitate quick and efficient review by Highmark’s Utilization Management team․ Proper completion of the form helps avoid delays and ensures that patients receive the necessary treatments promptly․ The form is available online for easy access and submission, making the prior authorization process more convenient for healthcare providers․
Where to Find the Highmark Prior Authorization Form
The Highmark Prior Authorization Form PDF can be easily accessed through Highmark’s official website․ Providers and patients can navigate to the “Forms” or “Resources” section, where the document is available for download․ Additionally, Highmark offers the form through its provider portal, ensuring convenient access for healthcare professionals․ For those who prefer alternative methods, the form can also be obtained by contacting Highmark’s customer service or Utilization Management department directly․ Some providers may access the form via fax by requesting it from Highmark’s dedicated fax line․ Highmark also provides the option to submit the form electronically through their online submission platform, streamlining the process for providers․ Ensuring you use the correct and most recent version of the form is crucial to avoid delays in the approval process․

Submission Process
The Highmark Prior Authorization Form PDF can be submitted by fax or by calling the Behavioral Health team․ Providers will receive a reference number upon notification of submission․
How to Submit the Highmark Prior Authorization Form
The Highmark Prior Authorization Form can be submitted via fax or by contacting the Behavioral Health team․ For fax submissions, ensure each form is faxed separately and completed legibly in black or blue ink․ When calling, have the patient’s details, service information, and medical justification ready․ Upon submission, a reference number will be provided for tracking purposes․ This number is essential for follow-up inquiries․ The process is designed to be efficient, with options to suit different provider preferences․
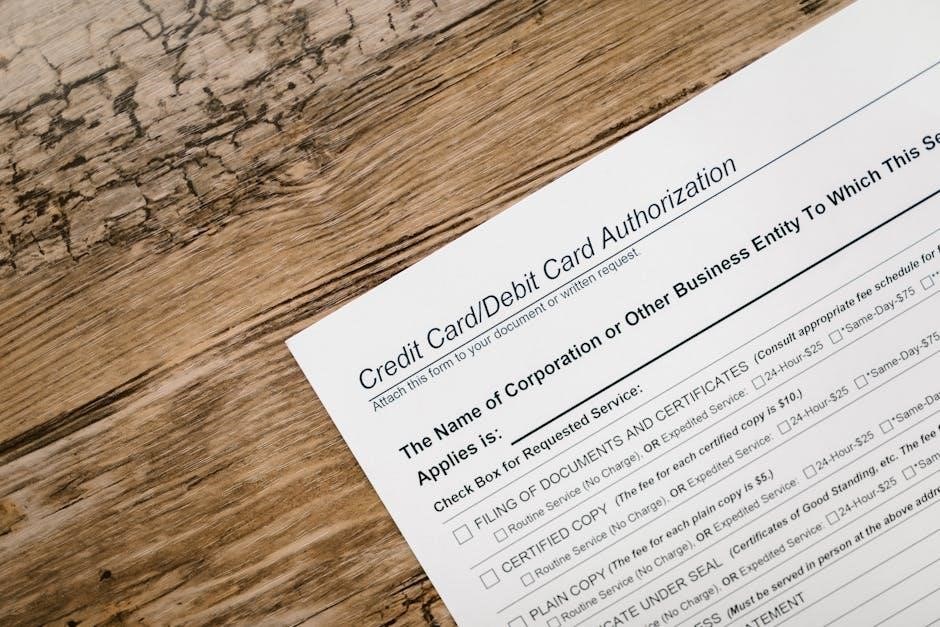
Required Information for Completing the Form
To complete the Highmark Prior Authorization Form, specific details are necessary to ensure timely processing․ Providers must include the patient’s full name, date of birth, and insurance identification number․ Accurate service or drug information, such as the procedure code (CPT code) or medication name, is also required․ A clear medical justification for the requested service or treatment is essential, detailing the patient’s condition and rationale for the authorization request․ Additional documentation, like medical records or test results, may be needed to support the request․ Providers should also include their contact information and credentials for verification purposes․ Ensuring all fields are filled legibly and completely helps avoid delays․ A reference number will be provided upon submission for tracking purposes․

Prior Authorization Requirements
Prior authorization is required for specific services or drugs to ensure they are medically necessary and cost-effective․ Highmark mandates this process to promote quality care and manage healthcare expenses effectively․
When is Prior Authorization Necessary?
Prior authorization is necessary when specific medical services, treatments, or medications require pre-approval to ensure they are medically appropriate and cost-effective․ This process typically applies to high-cost drugs, specialized procedures, or non-emergency services․ For example, certain imaging services like MRI scans or brand-name medications may require prior authorization․ Highmark mandates this step to verify that treatments align with clinical guidelines and patient needs; Providers must submit a prior authorization request before rendering certain services to avoid reimbursement issues․ Patients should check if their procedure or medication requires this approval by entering the CPT code on Highmark’s website or consulting their healthcare plan․ This ensures seamless coverage and avoids delays in care․
Common Reasons for Prior Authorization Requests
Common reasons for prior authorization requests include the use of high-cost medications, specialized treatments, or non-emergency procedures․ Highmark often requires pre-approval for brand-name drugs when generic alternatives are available․ Additionally, certain medical devices, imaging services like MRIs, and surgical procedures may need authorization․ This ensures that treatments are medically necessary and align with clinical guidelines․ Providers must submit detailed clinical information to justify the request․ Patients should check Highmark’s requirements by entering the CPT code online․ This process helps control healthcare costs while ensuring patients receive appropriate care․ By verifying the necessity of treatments upfront, prior authorization promotes efficient and effective healthcare delivery․

